Healthcare: Vicious politicization and vaccination failure
Oleg Monastyrsky-Severny
Summary
In 2021, the health care system of Belarus showed poor effectiveness in responding to COVID-19 pandemic challenges, both in preventing deaths and vaccination. Important managerial decisions were often made based on political expediency, rather than health support considerations.
The practice of concealing health care problems became common. Many professionals who raised questions were forcedly silenced. The strengthened administrative control and regulation triggered an outflow of specialists, although the salaries in the industry were the highest in the previous few years, mainly through bonuses paid to those who directly worked with COVID-infected patients.
The vaccination campaign failed due to the ineffective awareness-building efforts of the Health Ministry and general vaccination hesitancy amid the increased coronavirus incidence and shortages of medicines and consumables.
Trends:
- Elimination of vertical communication channels within the system, purges of undesirable personnel, and fear-mongering;
- Brain drain and demotivation of those who stayed, as a consequence, which affects the quality of medical care and medical science;
- Manipulations of statistics for creating a sense of self-complacency in one part of society and emotional discomfort in the other part that did not trust official data;
- Erosion of credibility of the state health care system, complicated communication between doctors and patients;
- Ineffective awareness-building efforts of the Health Ministry during vaccination.
COVID-19 pandemic as a challenge to the health care system
The global COVID-19 pandemic continued in 2021 in the so-called “second” (winter 2020–2021 in Belarus) and “third waves”. In Belarus, the third wave began in April and peaked in October when the delta variant of the coronavirus infection came to the country, bringing twice as high contagiousness and more frequent severe forms of the disease, including in young patients.
The increased contagiousness of the new SARS-CoV-2 variant and the larger number of severe forms were yet another significant challenge to global health care in terms of available treatment and technological capacities, increasingly requiring oxygen supply, health monitoring equipment, etc. In some countries (including Russia), hospitals got so quickly overcrowded with patients, and the media began to describe the situation as catastrophic.
Various vaccines were developed surprisingly quickly and the worldwide vaccination campaign began, being, in fact, another challenge to the national health care systems.
Incredibility of Belarusian COVID-19 morbidity and mortality statistics
The coronavirus pandemic (like any acute respiratory viral infections) came in waves with different morbidity rates. However, the data provided by the Ministry of Health of Belarus on a daily basis were significantly different from those of the neighboring countries, and often went beyond the bounds of common sense.
The Oxford University Our World in Data provides a good visualization of SARS-CoV-2 pandemic waves. Figure 1 shows the dynamics of the number of patients with COVID-19 (based on PCR tests) in Belarus and the neighboring countries.
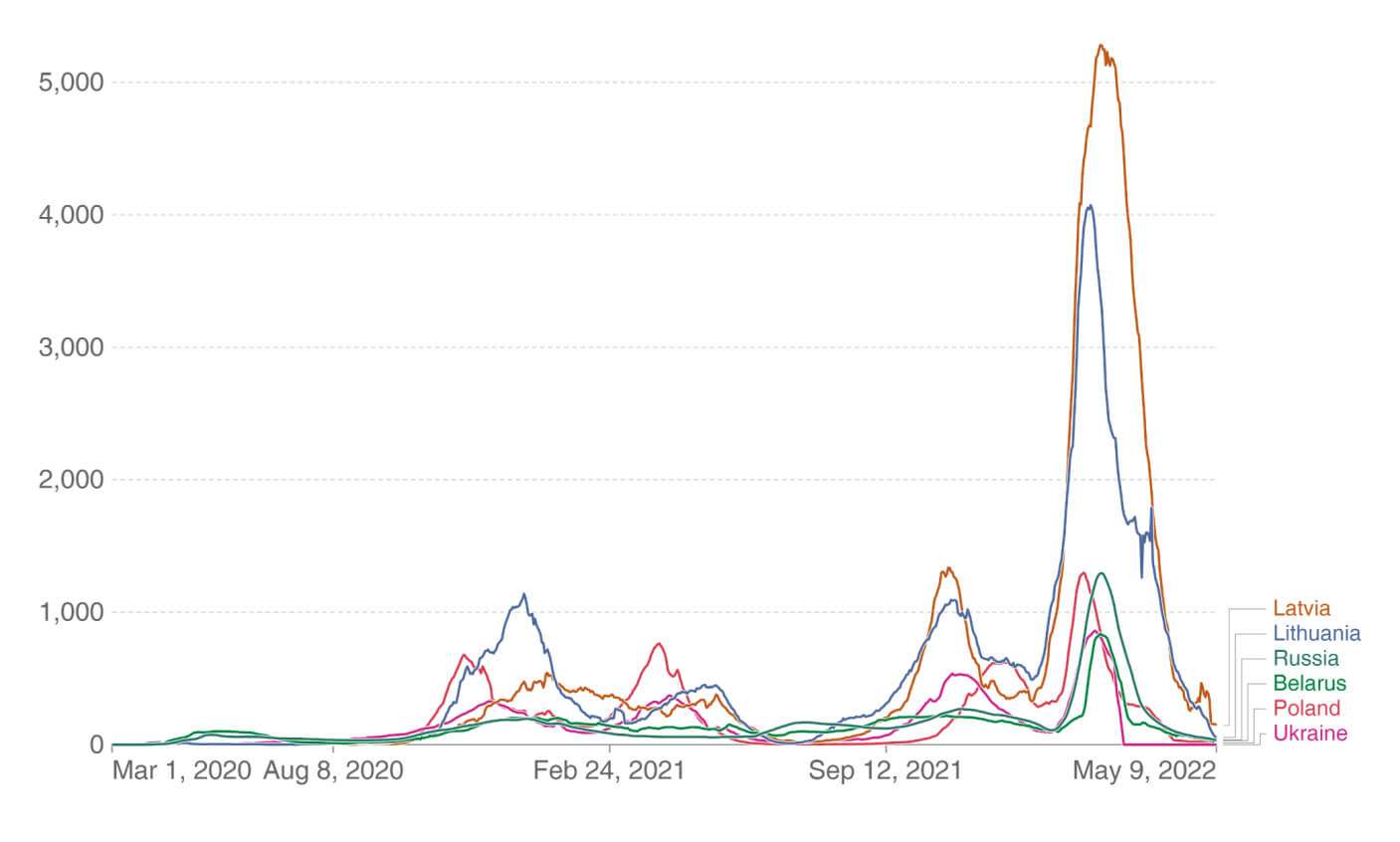
Figure 1. Daily new confirmed COVID-19 cases per million people
Note. 7-day rolling average. Due to limited testing, the number of confirmed cases is lower than the true number of infections.
Source: Our World in Data.
Conspicuously, Belarus and Russia differ from other countries by the unusual smoothness of these waves, which means that the number of officially reported cases is lower. At the beginning of the year, First Deputy Minister of Health Elena Bogdan said that “the coronavirus incidence plateaued in Belarus”. This could be a good meme, but not a clear epidemiological term.
This “plateau” probably resulted from the limited possibilities to perform PCR diagnostics in Belarus. There are significant reasons to doubt this, though, and to believe that the line agencies and/or the central government decided not to provide the real data. Below are arguments in a nutshell in favor of this assumption.
An extrapolation of the data of the spring survey by SATIO and BEROC shows that as of early March 2021, more than 1.2 million of the urban population aged 18 to 64 had been exposed to the COVID-19 virus in the past,1 while according to the Ministry of Health, there were almost half as many such persons (697,600) as of the end of 2021.2
The national statistics on the number of deaths from COVID-19 in Belarus (Figure 2) was also phenomenal. The deceased were even called differently: those died with detected coronavirus infection (5,561 as of the end of 2021). Their number virtually did not change throughout the epidemic waves, which contradicts all the laws of epidemiology, let alone the mathematical logic.
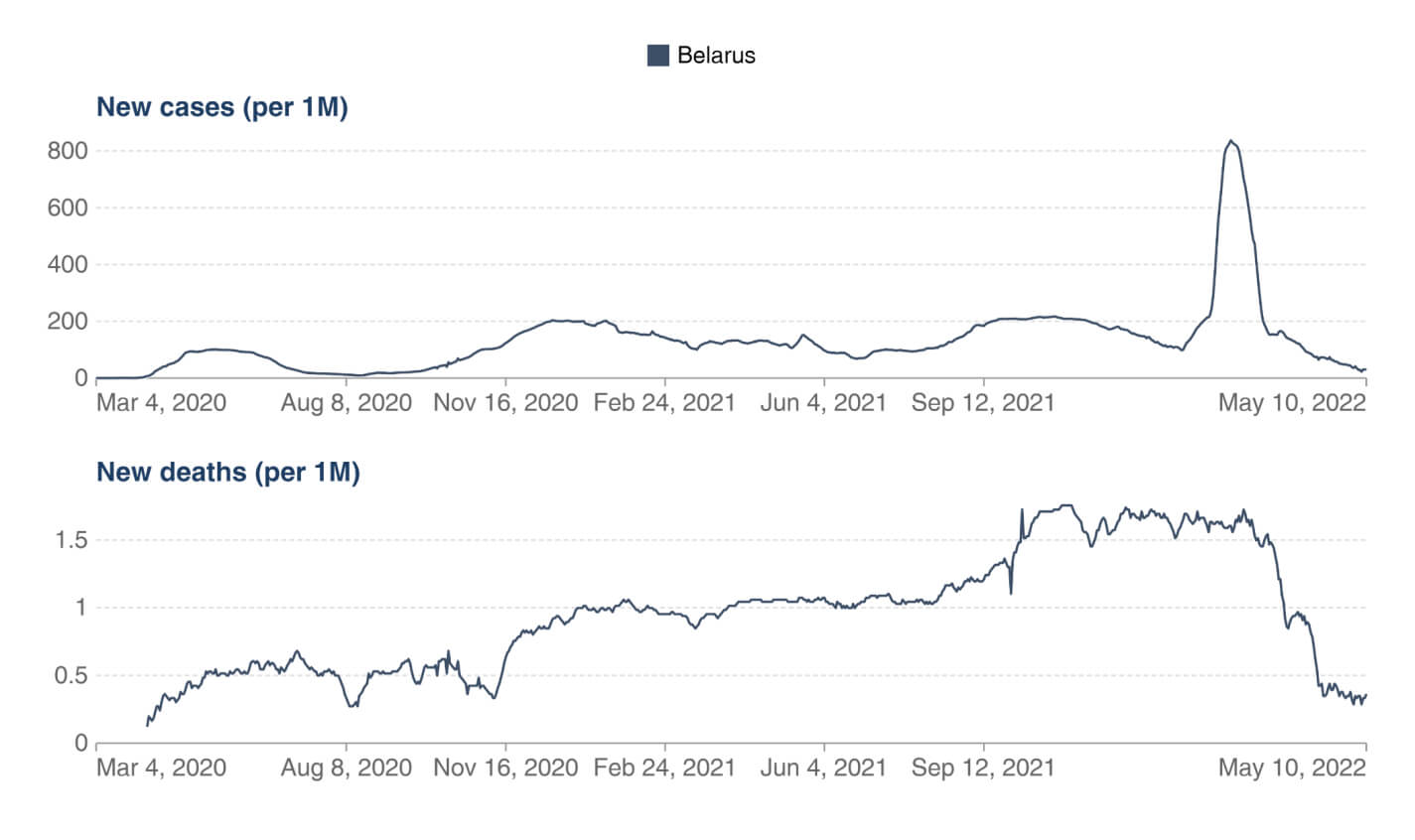
Figure 2. Daily new confirmed COVID-19 cases & deaths per million people
Note. 7-day rolling average. Limited testing and challenges in the attribution of cause of death means the cases and deaths may not be accurate.
Source: Our World in Data.3
The comparison of Belarus with the neighboring countries with respect to the same parameters helps visualize this phenomenon (Figure 3).
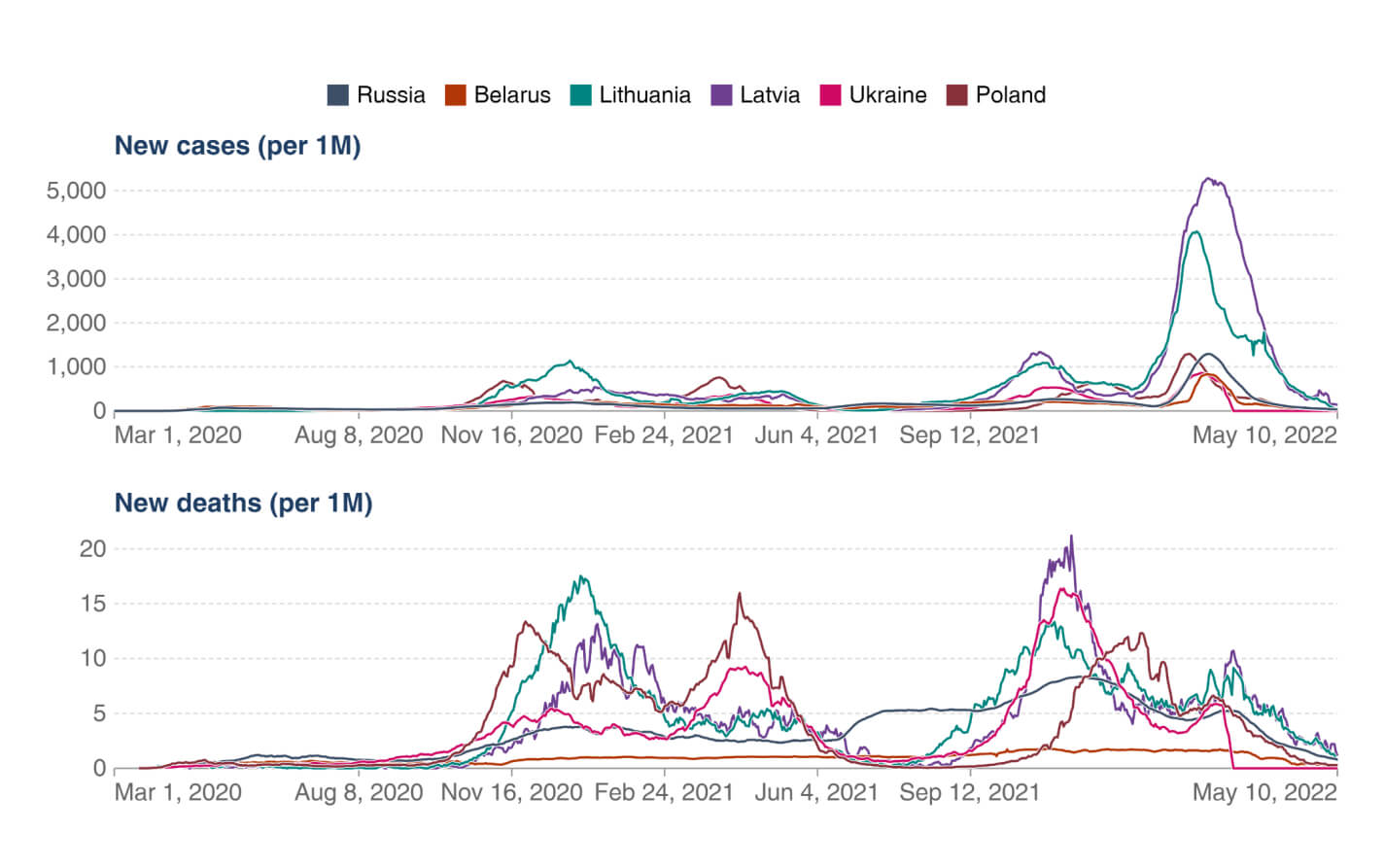
Figure 3. Daily new confirmed COVID-19 cases & deaths per million people
Note. 7-day rolling average. Limited testing and challenges in the attribution of cause of death means the cases and deaths may not be accurate.
Source: Our World in Data
In most countries, the number of deaths naturally increases with wave-like growth of morbidity, so the almost flat lines in Belarusian statistics look anomalous, and cannot be explained by other reasons, but an arbitrary decision to provide this particular information.
The real mortality rate could be estimated based on the excess mortality data, but these statistics have not been available since 2020, so it can only be estimated judging by indirect indicators. Nature journal published research conducted by American and Belarusian experts, who used a validated mathematical model of the analysis of Google requests for ritual services in the period from early 2020 to August 2021. According to the experts, during the studied pandemic period, mortality in Belarus exceeded the pre-pandemic values by more than one-third on average (2,953 to 3,690 excess deaths).4
eLife journal published an analysis of excess mortality5 based on the World Mortality Dataset, the largest and most regularly updated open database of mortality in 103 countries. Given the data on the first half of 2020 provided by Belarus to the UN Statistical Commission (5,700 deaths against 390 reported by the Health Ministry), the authors recorded a 14.7-fold underreporting. As one of the authors wrote, “it is hard to assume that so large underreporting can have any unintentional explanation”.6
Such manipulation of statistics creates a false sense of self-complacency for one part of the population and chronic emotional discomfort for another, i.e. those who realize the apparent improbability of the given numbers. This undermines trust in official medicine, complicates communication between doctors and patients, impedes analysis of the real state of affairs in the industry, and the ability or willingness to make carefully weighed managerial decisions. Besides, the inaccessibility of mortality data, the silencing of the facts of coworkers’ deaths and lack of respect for them, and the apparent contradictions between the official data and the real situation significantly demotivated health workers.
Ineffective management as a scourge of the health care system
Problems with supplies of medicines and consumables continued in 2021. Although production of means of individual protection and antiseptics was launched after the first wave of the pandemic, there were mass interruptions of supplies of consumables for lung ventilators, anticoagulants, Remdesivir and other drugs.
Health Minister Dmitry Pinevich said that BYN 1.5 billion (around 1% of GDP7) were spent on COVID-19 response measures in 2021. BYN 273.5 million were also allocated from Lukashenko’s reserve fund, and the World Bank provided a USD 98 million loan under the program of emergency response to COVID-19 in the Republic of Belarus. For comparison, Lithuania allocated slightly over 1% of GDP8 in 2020 to support the health care system, and there were no significant disruptions of medicine supplies, although there were some difficulties with protective gears and antiseptics at the very beginning of the pandemic, but that was typical of all countries without exception.
The above undoubtedly rooted in the Belarusian authorities’ inarticulate policy, i.e. restrictive measures taken during the pandemic, the vaccination failures, ineffective financial management, and rigid funding of the health care sector, which complicated flexible planning and distribution of funds, including for preventive procurement.
Hospitals reported systematic oxygen supply failures, like it happened, for example, in the Vitebsk Emergency Hospital, where oxygen supply devices malfunctioned regularly and for long periods, putting patients at risk. The problem was not resolved at the local level, so head of the intensive care unit Vladimir Martov had to appeal to the minister of health. The case went public, and the Ministry of Health sent a commission to the hospital. The commission, however, checked how properly the patients were treated, rather than looking into the oxygen supply interruptions. Martov, a renowned specialist with a thirty-year experience, was fired, and problems with oxygen continued. Doctors of other hospitals pointed at the same problems and the similar approach to solving them.
Politicization of health care management and vaccination failure
In 2021, top officials of the country fundamentally changed the rhetoric regarding the relevance of COVID-19 related topics for Belarus, and began using the pandemic as an occasion to demonstrate the state’s concern for its citizens, while hospitals and polyclinics became a background for TV reports about the red zones. SB Belarus Today newspaper counted about twenty such statements made by Lukashenko alone during the year.
However, the demonstration of the high attention to the problem did not lead to an increase in the effectiveness of the system, but only exacerbated the dominating considerations of political expediency and voluntarism in managerial decision-making. For example, during the next wave of the pandemic in October, Lukashenko criticized the compulsory wearing of masks, after which the Ministry of Health issued decree No.111 that abolished the administrative responsibility for not using respiratory protection indoors and in public transport.
The government made the political decision not to import Pfizer, Moderna, and AstraZeneca vaccines to Belarus, although, according to a SATIO/BEROC opinion poll, the population trusted them more than the available Russian Sputnik V and Chinese Sinovac. In the autumn, Svetlana Tikhanovskaya’s Office negotiated with the European Union a donation of at least one million doses of European vaccines to Belarus,9 but Minsk ignored the offer.
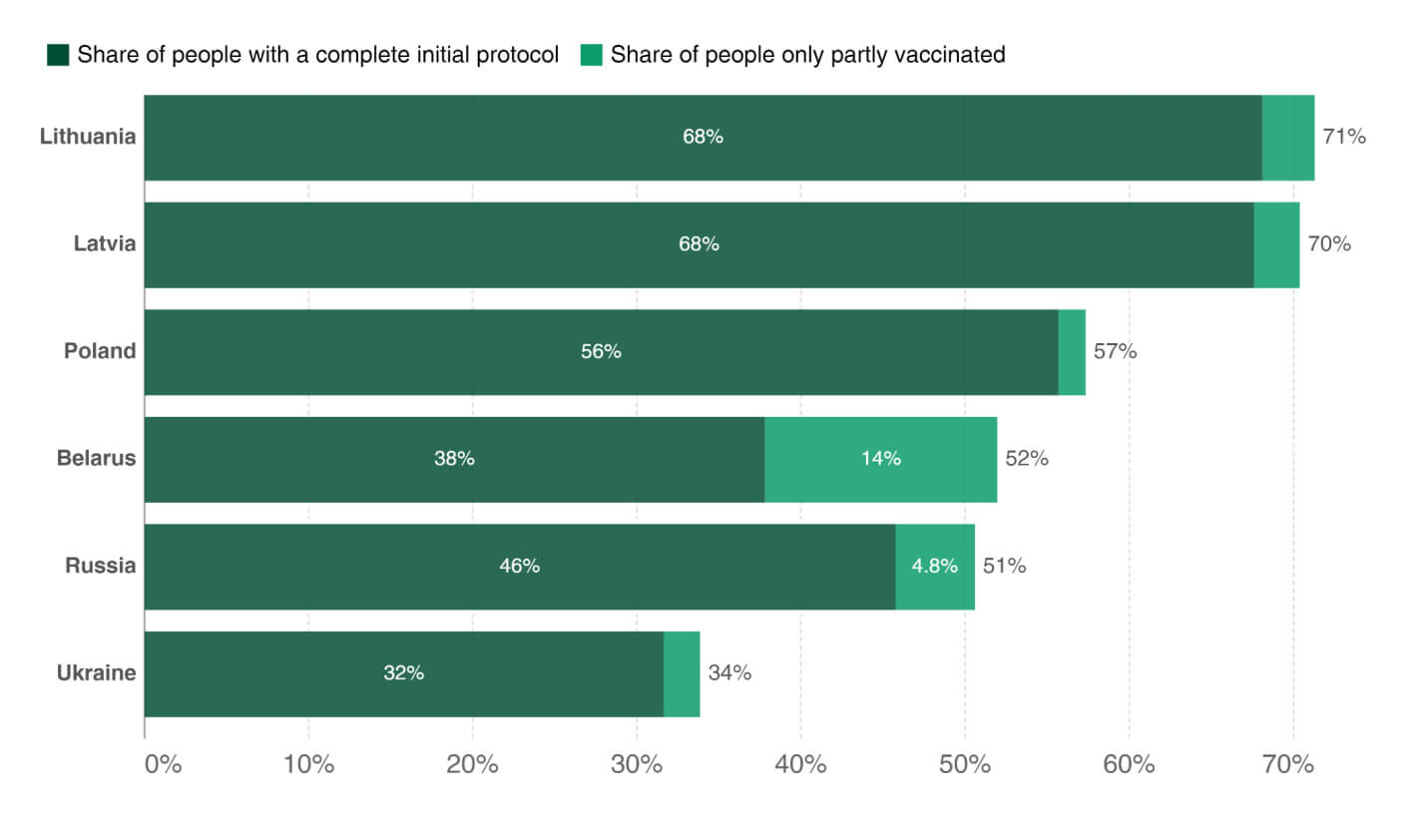
Figure 4. Share of people vaccinated against COVID-19, Dec 31, 2021
Note. Alternative definitions of a full vaccination, e. g. having been infected with SARS-CoV-2 and having 1 dose of a 2 dose protocol, are ignored to maximize comparability between countries.
Source: Our World in Data
The SATIO/BEROC opinion poll showed that more than a half of Belarusians were reluctant to get vaccinated, and one in four categorically rejected it. The authorities did not conduct an effective awareness building campaign. Lukashenko said that “the Russian and Chinese vaccines proved to be much better than their Western analogues”. As a result, by the end of 2021, 51.8% of the population of Belarus10 received one vaccine dose, and only 39.8% completed a full course of vaccination, which was a considerably lower rate than in Poland and Lithuania (Figure 4).
Personnel purges and nursing staff shortages
In 2020, politically motivated dismissals of health professionals (especially healthcare administrators) were rather sporadic and were primarily targeted at the most visible undesired persons, such as Professor Alexander Mrochek, former director of the Cardiology Research Center, while in 2021, the purges became massive and systematic.
According to the Medical Solidarity Foundation of Belarus and open sources, as of November 2021, more than 90 health professionals were fired on political grounds, including, for example, Mother and Child Center cardiologist Elena Baranova after 25 years of work for her comments on Facebook. The Foundation said that more than 250 health care workers were arrested and/or fined.11 Subsequently, most of them were also fired. Their contracts were not extended, which, formally, can be done by the employer under the applicable law.
Seven health care workers were behind bars on criminal charges (and some more were released on their own recognizance), and at least eight medical students were expelled from universities. In November, undergrad student Vladislav Martinovich was expelled from the Belarusian State Medical University, and sentenced to four years in prison for administering White Coats Telegram channel, which was declared extremist.
This “decimation” during the pandemic could not but jeopardize the quality of health care and demotivated health workers, making them think about leaving Belarus or switching to other trades (in particular IT). It is not surprising that in 2021, even according to the official statistics, the medical service density reduced from 55.8 to 55.2 per 10,000 population; nursing staff – from 134.1 to 120.7.
It is planned to solve the staffing problem, applying old methods, i.e. by increasing the number of targeted vacancies in higher educational medical institutions to 80%, and the admission itself by 160 enrollees in medical universities and by 300 in nursing schools. Also, the authorities are counting on the attractive salaries (153% of the national average for doctors and 93% for nurses), but do not take into account that to earn this money, doctors need to work 37% more hours, and nurses 26% more hours on average. Besides, the average salary includes bonuses for treating Covid patients, which will no longer be paid once the pandemic is over. But even during the pandemic, not all health care workers received the bonuses, and most of them had much more modest incomes.
Conclusion
The transformation of Belarusian society and the state in 2021 resulted in a transformation of the Belarusian health care system into an outer show, convenient for the bosses, but problematic from the point of view of efficiency. The elimination of vertical communication, repressions, and personnel appointments based on political loyalty made health care ineffective and formalistic on the part of the staff.
Since the current state system is predominantly punitive and repressive, it is safe to assume that the staff attrition will increase, which means that the quality of medical care services will continue to decline in many respects due to deterioration of the material resources and pay cuts. Also, the toxicity of Belarus as a state will inevitably lead to a limitation of contacts with the civilized world, which will affect health care quality even more and lower the already low level of medical science.
On top of this, virtually no efforts were made to digitalize health care in 2021, although it had been previously declared a panacea for all woes. It was only reported in March that the Ministry of Health discussed a project on a software platform for the centralized health information system in Belarus. Meanwhile, Belarus is to start repaying in 2022 the funds borrowed from the International Bank for Reconstruction and Development for this digitalization.
The manual steering of the system will increase, and performance discipline (in practice, simulation of vigorous activity) will be further named among the priorities against the backdrop of the reduced financing of the industry. It will be necessary to find additional resources to keep health care alive, which, in the situation of dropping revenues from the export of services, can be only compensated by an increase in the share of fee-based services in state clinics and hospitals. Ultimately, the quality of medical care will deteriorate even more.